Chakib Jaber
Chief Technology Officer
SpinSys
Electronic health information exchanges, more commonly referred to as HIE, are designed to allow healthcare providers and patients the ability to access and share each patient’s medical information securely and electronically. This system is intended to improve the speed and safety of providing patient records to necessary doctors, nurses, pharmacists and even the patient, all while lowering the ever-mounting costs of healthcare.
Information Exchange and Standardization of Care
Despite the implementation of electronic health records (EHR) in many medical practices, many patients’ medical records remain stored on paper in filing cabinets and boxes. However, the process of converting to electronic health records has slowly been increasing over the past several years, providing medical data that can be securely shared between physicians, facilities, analysts with a goal to improve the quality of patient care.
However, with the growth of vendors implementing solutions to support electronic medical records exchange, the need for standardization continues is becoming the approach that the industry is following in order to allow for multiple systems to share data. As an example, one of the main purpose of collecting patient data electronically is to make it available to the patient and to all of the patient’s healthcare providers, those individuals and facilities must be able to communicate by using similar codes and specifications in order for the data to be accurate understood and applied by all.
For example, if Patient A undergoes laboratory testing and imaging for a single ailment, Patient A will receive results and data from both the laboratory and radiology departments of his local facility. When those two departments input these results into the health information exchange, those results should be organized and reported similarly so that both departments, as well as Patient A’s primary physician and Patient A, can understand the data and create an appropriate treatment plan.
The challenge is that the laboratory probably has one application for entering data, and the radiology department has a completely different system. This makes it very difficult for all of the healthcare providers to gather and compare information when the same information, such as about Patient A’s medical history, is stored in a different place and under different titles. These disparities can add challenges across multiple levels, from system integration to doctors/nurses trying to interpret the data which can lead to increase cost and time to interpret and analyze the data, effecting the quality of care for patients. Moving toward standardized applications, data sharing and common analytics in the information exchange is the next logical step that the industry is taking in the electronic health records movement.
The Implementation of Fast Healthcare Interoperability Resources (FHIR)
Health Level Seven International (HL7) was developed and adopted by the American National Standards Institute (NSI) to be the protocol for clinical and administrative data. HL7’s goal was to improve patient care while optimizing healthcare workflow, so it included a number of standards and guidelines by which healthcare systems were directed to communicate with each other.
However, HL7 was focused mainly on a message-based system that required each provider or facility to customize its own site. This customization by individuals led to inconsistencies in naming and other semantic issues between providers, creating more misinformation and medical errors.
Recognizing these issues HL7 eventually took on the license of Fast Healthcare Interoperability and Resources (FHIR), a program that provided a more standardized approach to healthcare data. Clinical resources are defined in concrete terms, such as “Medication Prescription,” “Procedure” and “Condition.” When healthcare providers fill in each of these resources in real time, they are easily transferred to other providers without misinterpretation.
In addition, the new resources are streamed to a data store to be correlated with other analytic data, giving healthcare officials the opportunity to track epidemics, detect prescription drug fraud and even determine service information such as emergency room wait times.
The Evolution of Substitutable Medical Applications and Reusable Technologies
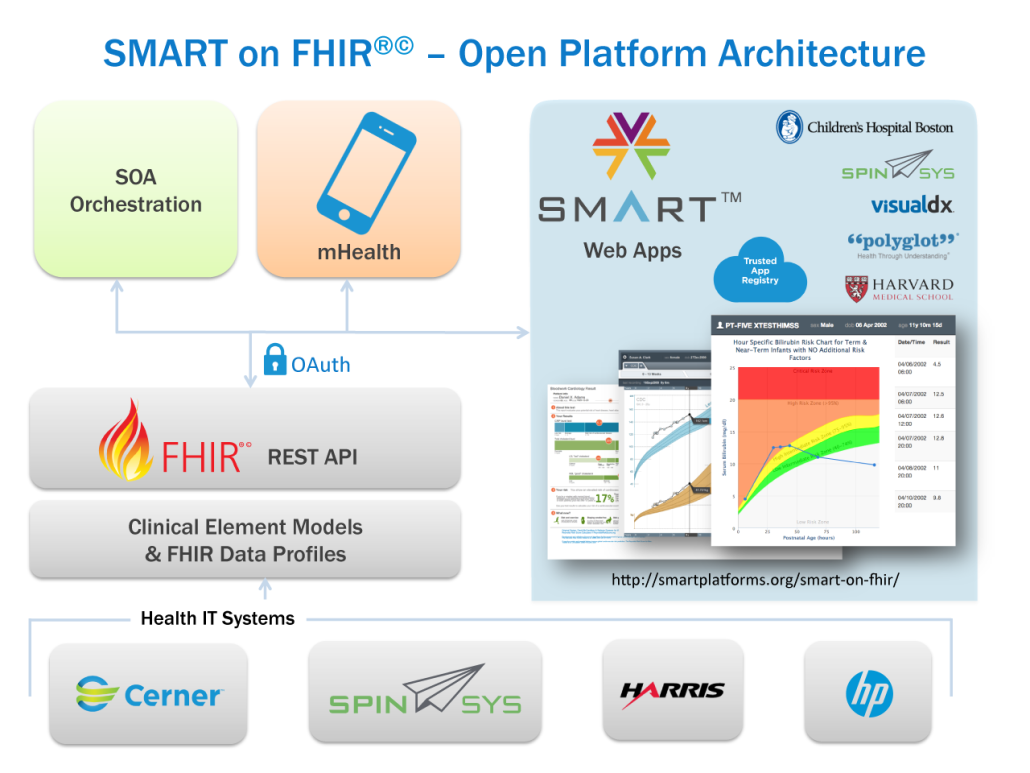
As the data-standards-based programs of Fast Healthcare Interoperability Resources continued to be adopted, local healthcare providers and physicians complained that not all of the resources were applicable to their practices and were therefore cumbersome. Members of the medical teams at Harvard Medical School and Boston Children’s Hospital worked closely with the healthcare industry in developing Substitutable Medical Applications and Reusable Technologies, or SMART, in addition to leveraging First Healthcare Interoperability Resources system which coined the industry term “SMART on FHIR”.
Taking a cue from mobile technology developers, the new system is focused on providing a set of standards for third-party applications. This means that medical application/analytics developers can continue to construct their records systems with many different appearances and styles, but the semantics of health record profiles as well as data sharing leverage common standards. These constraints include terminology restrictions, data type restrictions and hierarchical structuring of resources.
By requiring particular semantics and organizations structures from systems that share health records and enforce standardization of data collection while allowing individual healthcare providers to exchange health data in a manner that best reflects their technology stack and well as their business processes and workflow needs.
SMART on FHIR Adoption by EHRs and HIEs
Substitutable Medical Applications and Reusable Technologies (SMART) has gained a lot of traction since its introduction in 2010. Prominent EHR vendors such as Cerner, Harris Corporation and athenahealth have developed applications that could plug into the system and be integrated cleanly into clinical workflow. In addition HIE solution integrators, such as SpinSys, have begun leveraging SMART and FHIR as part the solution offerings to facilitate the re-use and ease of integration of solutions across multiple EHR and HIE based solutions.
In fact, each EHR company that participated found a way to create a functionality radically different from the other vendors. For example, Cerner focused on patient demographics, determining which apps would be most useful and desired by individual patients. On the other hand, Harris Corporation decided to showcase real-time inquiries that combined patient queries from the system servers to generate more complete patient records. These are just two examples of differing apps that were designed and that worked with the separate EHRs while still using Substitutable Medical Applications and Reusable Technologies and Fast Healthcare Interoperability Resources.
The technology also allows individuals to create their own apps, encouraging providers who do not see what they want not to wait for it to be developed. This ability to create personalized apps is both empowering for healthcare providers and an impetus for many health Information exchange providers to work harder and faster on developing purchasable apps that providers will want.
Implications for the Health Information Exchange
Although they all seem disconnected in their development and interoperability, EHRs, HIE, FHIR and SMART are working toward the same goal: standardizing patient data to improve patient care, reduce medical errors and lower operational costs.
Most healthcare providers are now entrenched in the process of converting to electronic patient records. However, a one-size-fits-all approach to gathering, storing and sharing that data will not work when there are so many different types of medical care and facilities. For example, the information required by a cardiologist’s office has some overlapping information used by the local pharmacy, but much of the data is provider-specific. Because of this specificity, using a single program is not feasible.
Likewise, patient data can easily be misinterpreted when different terminologies and organization structures make it difficult to compare and collect important reports.
The information storage of the future rests in the standardization of data semantics and the interoperability of different systems and apps. This is where the Health Information Exchange solution providers can leverage SMART on FHIR as one mechanism to pave the way to functional and efficient patient data exchange, that can lead the way to the quick development to a wide range of functional apps and analytics aimed at improving the quality of care.